HemoSphere Vita monitor
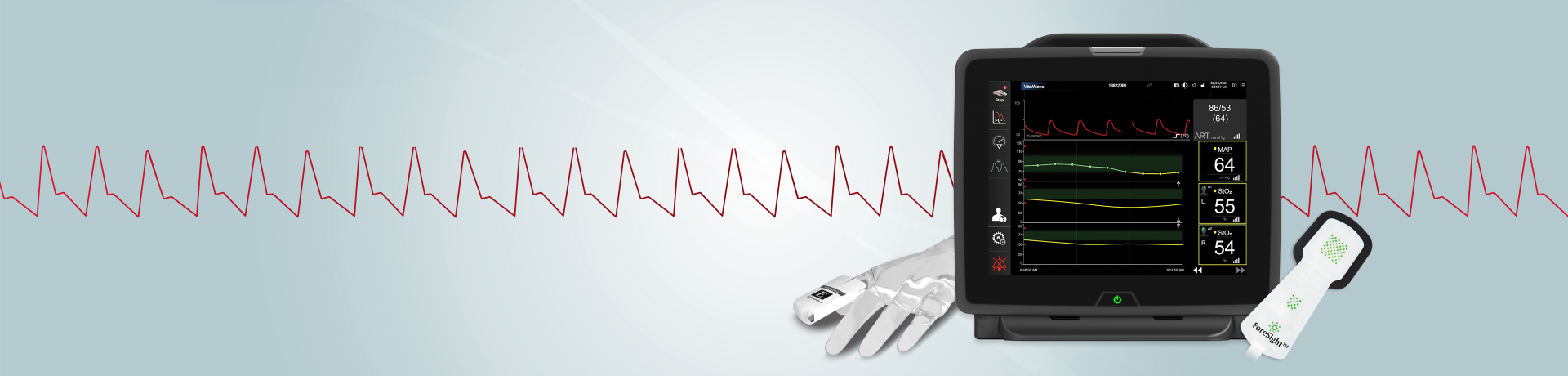
Inform your clinical decision-making with continuous noninvasive blood pressure monitoring
HemoSphere Vita monitor provides continuous noninvasive blood pressure and tissue oxygenation insights designed to support informed decisions and proactive interventions.
Continuous noninvasive blood pressure monitoring (cNIBP) has been demonstrated to help clinicians reduce hypotension by 90% during noncardiac surgery compared to intermittent oscillometric cuff monitoring.*1
Discover how continuous monitoring can help clinicians identify and respond to
hypotension.1,8-10

*Single-center randomized control trial with 242 noncardiac surgery patients where hypotension was defined as time-weighted average (TWA) MAP < 65 mmHg during surgery.
**When compared to intermittent oscillometric cuff monitoring

Access continuous insights

With VitaWave finger cuff you can:
- Access continuous noninvasive blood pressure trends
- Leverage real-time monitoring to detect hypotension earlier than an intermittent oscillometric cuff
With ForeSight tissue oximetry sensor you can:
- Recognize and reverse cerebral desaturations
- Gain insights that help you maintain brain health and detect distal limb ischemia

IOH may elevate risk*2-4
Intraoperative hypotension (IOH) is common and often detrimental, even for younger and lower-risk patients,** and it can easily be missed with an intermittent oscillometric cuff. Even short periods of IOH are associated with significant postoperative adverse events such as myocardial injury (MI), acute kidney injury (AKI) and mortality.5-7
*IOH is defined as MAP <65 mmHg, a common definition
**According to a multi-center cohort study where younger and low-risk were defined as patients in the 18-40 age range.
Reduce both the incidence and duration of IOH*
With VitaWave finger cuff, you gain access to continuous, noninvasive blood pressure (cNIBP) monitoring.
cNIBP detects changes earlier than intermittent oscillometric cuff monitoring, which may enable you to identify hypotension and intervene sooner, potentially reducing hypotension complications for more patients.1,8-10

*When compared to intermittent oscillometric monitoring.

Know the risks: IOH
*According to a retrospective analysis where hypotension was defined as a MAP <65 mmHg for a cumulative duration of 15 min.
Recognize and reverse cerebral desaturations
Research has consistently shown that cerebral tissue oxygen desaturations are common, yet treatable. Reversing or avoiding cerebral desaturations has been shown to reduce incidence of cognitive impairment,15 ICU stay16 and hospital stay.17
ForeSight sensor delivers continuous, absolute StO2 readings where preinduction baselines are optional – while still giving you the freedom to set treatment thresholds and trend from a patient baseline.
Faster access and actionable data
HemoSphere Vita monitor with VitaWave finger cuff is designed for rapid setup and streamline ease of use, enabling you to individualize care for a wide range of patients and procedure types.
- Streamlined, rapid setup which can help you start monitoring quickly in critical situations
- Faster and easier to set up than arterial line monitoring
- Offers quick access to continuous blood pressure insights
Advance patient care with ongoing education
Edwards Lifesciences is here to help you stay on top of the latest clinical challenges.
Request a demo
References
- Kouz K, Weidemann F, Naebian A, Lohr A, Bergholz A, Thomsen KK, et al. Continuous finger-cuff versus intermittent oscillometric arterial pressure monitoring and hypotension during induction of anesthesia and noncardiac surgery: the DETECT randomized trial. Anesthesiology. 2023 Sep 1;139(3):298-308.
- Shah NJ, Mentz G, Kheterpal S. The incidence of intraoperative hypotension in moderate to high risk patients undergoing noncardiac surgery: A retrospective multicenter observational analysis. J Clin Anesth. 2020;66:109961.
- Gregory A, Stapelfeldt WH, Khanna AK, et al. Intraoperative hypotension is associated with adverse clinical outcomes after noncardiac surgery. Anesth Analg. 2021;132(6):1654-1665.
- Wesselink EM, Kappen TH, Torn HM, et al. Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth. 2018;121(4):706-721.
- Salmasi V, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney injury and myocardial injury. Anesthesiology. 2017;126(1): 47-65.
- Mascha EJ, et al. Intraoperative mean arterial pressure variability and 30-day mortality in patients having noncardiac surgery. Anesthesiology. 2015;123(1):7991.
- Wijnberge M, Association of intraoperative hypotension with postoperative morbidity and mortality: systematic review and meta-analysis. BJS Open. 2021;5(1):zraa018
- Maheshwari K., et al. (2018) ‘A randomized trial of continuous noninvasive blood pressure monitoring during noncardiac surgery’, Anesthesia & Analgesia, 127(2), pp. 424–431.
- Meidert A.S., et al. (2017) ‘The impact of continuous non-invasive arterial blood pressure monitoring on blood pressure stability during general anaesthesia in orthopaedic patients’, European Journal of Anaesthesiology, 34(11), pp. 716–722.
- Chen G., et al. (2012) ‘Impact of noninvasive and beat-to-beat arterial pressure monitoring on intraoperative hemodynamic management’, Journal of Clinical Monitoring and Computing, 26(2), pp. 133–140.
- Silver SA, et al. The economic consequences of acute kidney injury. Nephron. 2017;137(4):297301.
- Hobson C, Ozrazgat-Baslanti T, Kuxhausen A, et al. Cost and mortality associated with postoperative acute kidney injury. Ann Surg. 2015;261(6):1207-1214.
- Collister D, et al. Health care costs associated with AKI. Clin J Am Soc Nephrol. 2017;12(11): 1733-1743.
- Alshaikh HN, et al. Financial impact of acute kidney injury after cardiac operations in the United States. Ann Thorac Surg. 2018;105(2):469-475.
- Colak Z, et al. Influence of intraoperative cerebral oximetry monitoring on neurocognitive function after coronary artery bypass surgery: a randomized, prospective study. Eur J Cardiothorac Surg 2015 Mar;47(3):447-54.
- Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I, et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104:51-58
- Goldman S, Sutter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum. 2004;7(5):E376-81.
Medical device for professional use
Medical device for professional use
For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).

