IOH is common1,2,6
88%* of non-cardiac surgery patients (19,446/22,109) monitored with an arterial line experienced at least one hypotensive event* for at least 1 minute.1

88%* of non-cardiac surgery patients (19,446/22,109) monitored with an arterial line experienced at least one hypotensive event* for at least 1 minute.1

A wealth of evidence suggests a link between IOH and the increased risk of adverse outcomes – including MI, AKI, and mortality – after non-cardiac surgery.1,7,8
Acumen HPI software is effective in detecting haemodynamic instability and substantially reducing^ intraoperative hypotension. When used in surgical patients who require intraoperative haemodynamic monitoring during non-cardiac surgery.
^A single arm, multi-centre, prospective-to-historical control where non-cardiac surgical patients received arterial line monitoring.
*19,446/22,109 non-cardiac surgery patients. In a retrospective multicentre observational study that evaluated moderate-to-high risk (ASA status of 3 or 4) noncardiac surgery patients monitored for hypotension at hospitals that used an invasive arterial line ≥75% of the time. Hypotension/hypertensive event was defined as MAP <65 mmHg for at least one minute1
88%* of non-cardiac surgery patients (19,446/22,109) monitored with an arterial line experienced at least one hypotensive event* for at least 1 minute and the mean cumulative duration of IOH* was 28.2 minutes (standard deviation 42.6 minutes).1
88%* of patients (19,446/22,109) experienced at least one hypotensive event.*1

Mean cumulative duration of IOH* was 28.2 minutes (standard deviation 42.6 minutes).1
*From a retrospective multi-centre observational study that evaluated moderate- to high-risk (ASA status of 3 or 4) non-cardiac surgery patients monitored for hypotension at hospitals that used an invasive arterial line ≥75% of the time.1
Hypotension/hypotensive event was defined as MAP <65 mmHg for at least one minute.1

More than 1 in 12 patients (8 million people globally) over 45 years old experience MINS each year.10-12 In 2018, Sessler et al reported that MI was the leading cause of attributable postoperative death, accounting for 25% of all mortality.5
In non-cardiac surgery patients, research findings have revealed strong associations between intraoperative hypotension and elevated risk of both acute kidney injury (AKI) and myocardial injury after non-cardiac surgery (MINS).2-4

A 2017 study estimated 30-40% of all cases of AKI occur after surgery.13 Studies from 2015 and 2017 show associations between intraoperative hypotension and increased risk of acute kidney injury (AKI) in non-cardiac surgery.2,3
A large clinical study in 2015 found that post-surgery AKI was associated with:*
*From a retrospective, single-centre study that examined the impact of postoperative AKI in 50,314 moderate- and high-risk adult patients* undergoing surgery with ≥24-hour admission. Patients had no history of CKD, but likely were higher risk with more comorbidities vs patients who undergo outpatient or same-day inpatient surgery.14
In a systematic review of 42 papers,† elevated risk of postoperative myocardial injury, acute kidney injury, and mortality was reported when IOH dropped lower than 65 mmHg.8 Risk increased as blood pressure became progressively lower.8
†Studies evaluated the associations between IOH and at least one of 6 identified adverse outcomes among non-cardiac surgery.8

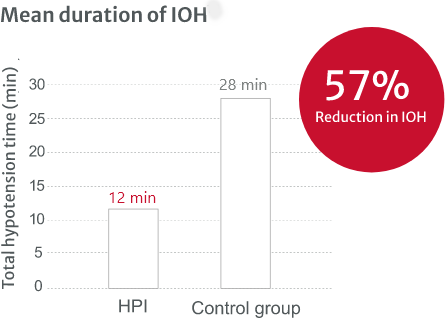
Acumen HPI is effective in detecting haemodynamic instability and substantially reducing* intraoperative hypotension. It is a first-of-its-kind intelligent decision support suite that provides clinicians with information regarding the likelihood of a patient trending toward a hypotensive event^, allowing proactive treatment.15,16
*A single arm, multi-centre, prospective-to-historical control where non-cardiac surgical patients received arterial line monitoring
^Hypotension/hypotensive event was defined as MAP <65 mmHg for at least one minute.

Acumen Hypotension Prediction Index software is unlocked with the Acumen IQ sensor or Acumen IQ cuff.
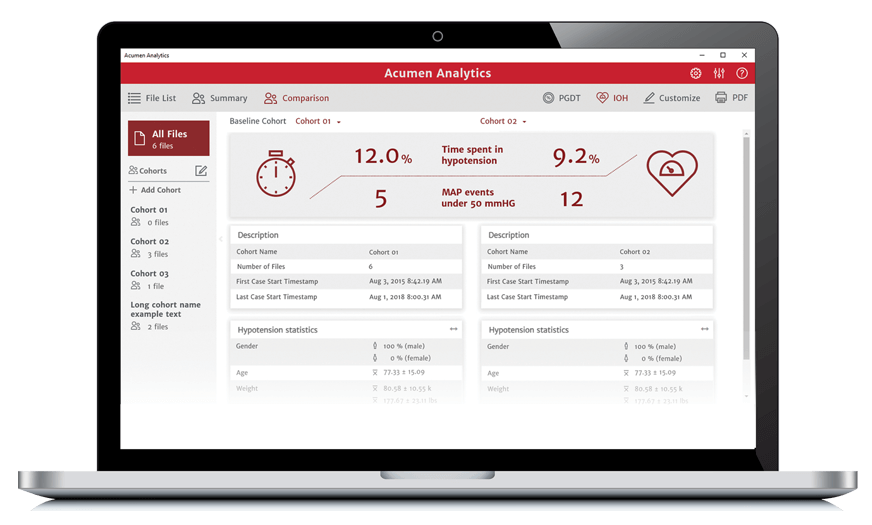
Acumen Analytics software enables you to retrospectively view and analyse haemodynamic parameters including mean arterial pressure, providing you insights into the frequency, duration, and prevalence of intraoperative hypotension in your practice.
With a long-term commitment to improving the quality of care for surgical and critical care patients through education, Edwards clinical education meets you no matter where you are in the learning process — with a continuum of resources and tools that continuously support you as you solve the clinical challenges facing you today, and in the future.
For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
We are committed to providing your institution, clinicians and staff with a high level of customer service and support to ensure seamless product implementation and ongoing use, including:
Monday through Friday, 8:00am to 17:00pm CET
