Shock is common
1/3 of ICU patients suffer some form of shock.3,4
Feb 22 is Heart Valve Disease Awareness Day — Learn more about the HVD symptoms at Listen to your Heart

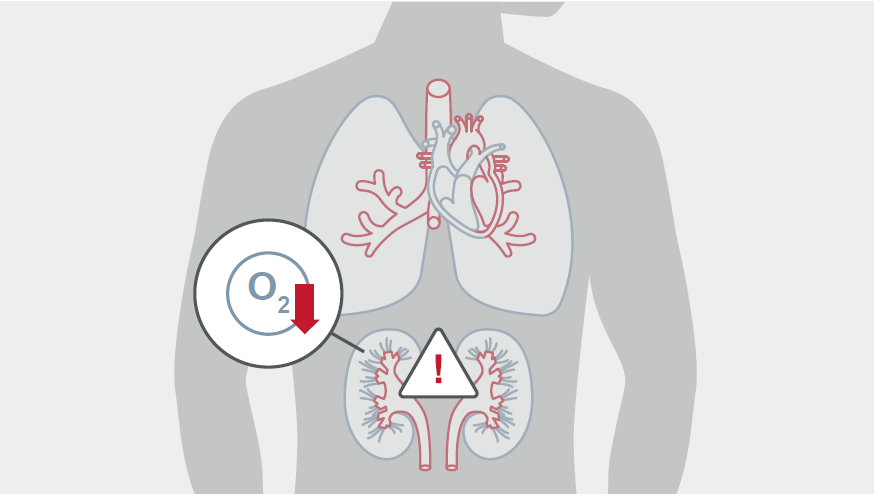
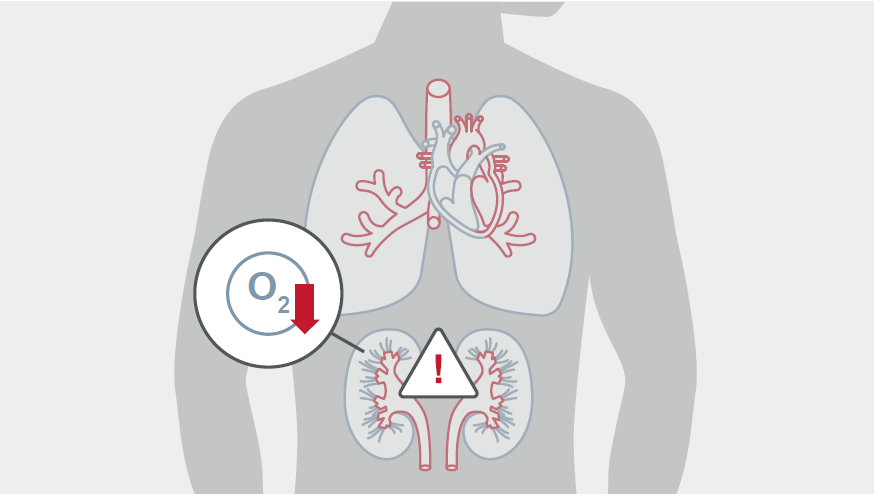
Shock, at its most basic level, is the inadequate delivery of oxygen to the tissues, which are dependent upon perfusion, pressure (MAP), and flow.1
1/3 of ICU patients suffer some form of shock.3,4

ICU patients presenting with shock have a nearly 40% risk of death.3
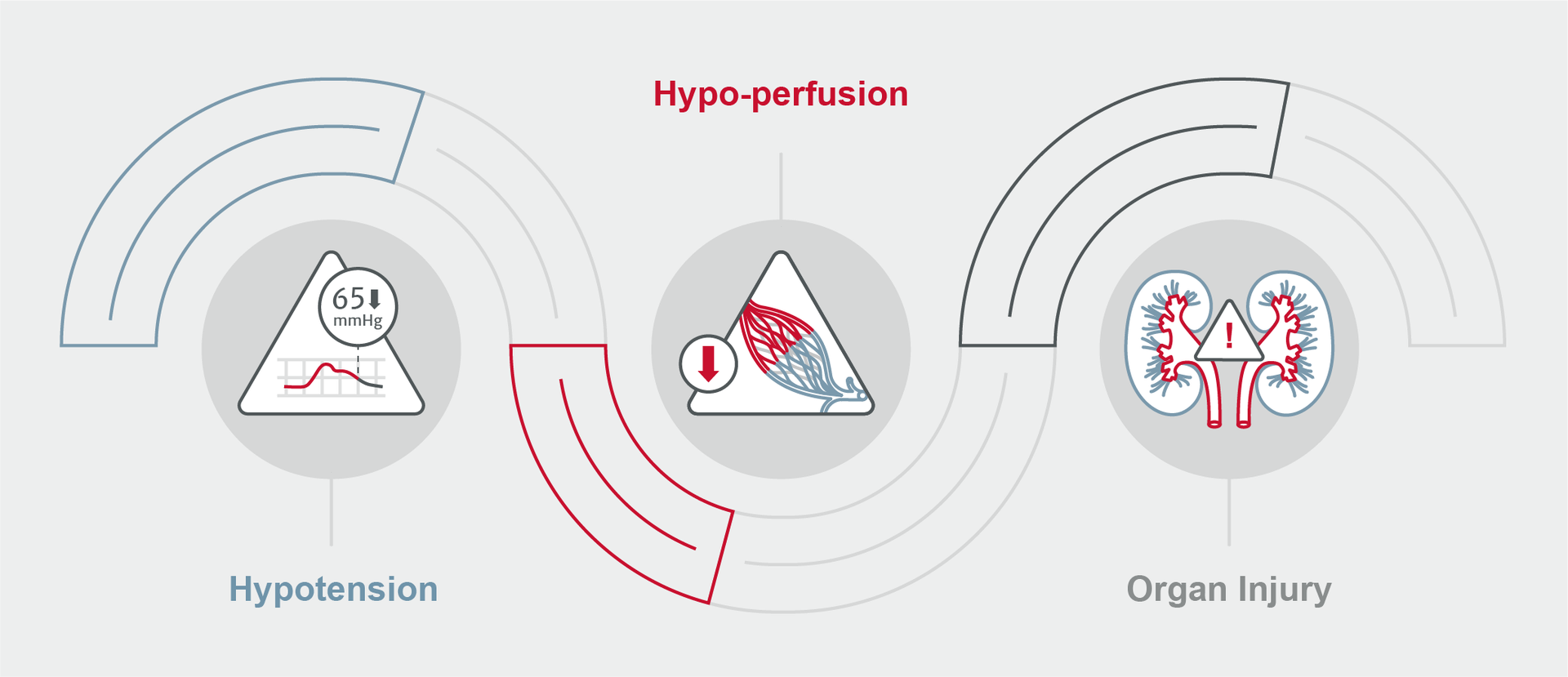
This deadly condition manifests through hypotension, hypo-perfusion, and organ injury.4
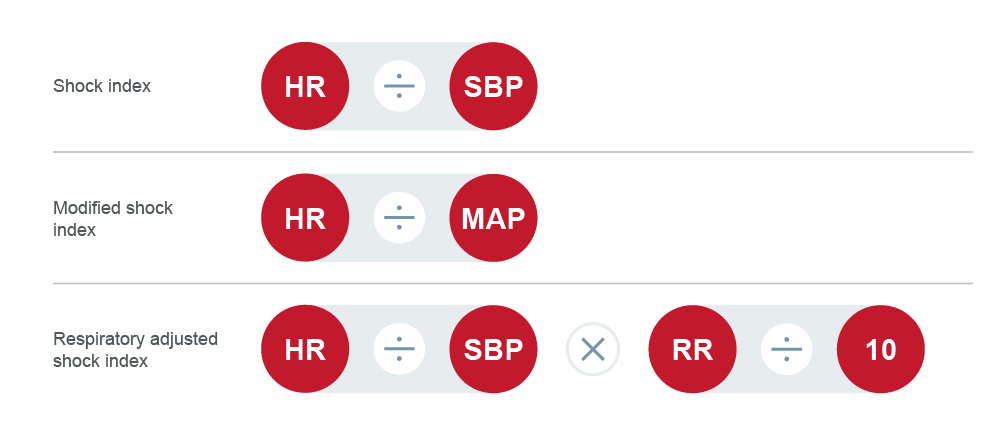
Modified shock index (MSI) has been shown to be a predictor of hospital mortality in critically ill and injured patients. There are other indices which may also be used to identify patients at-risk. Common indices:
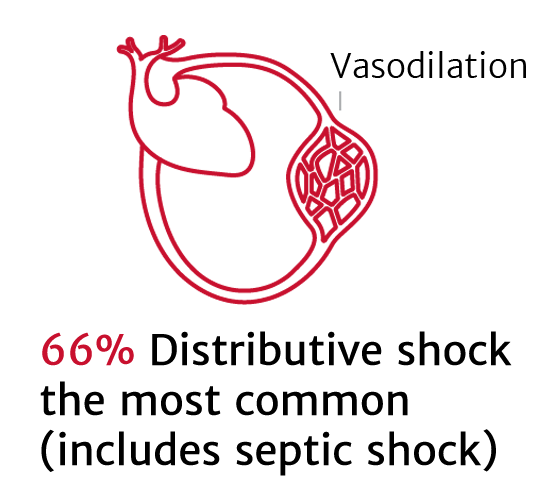
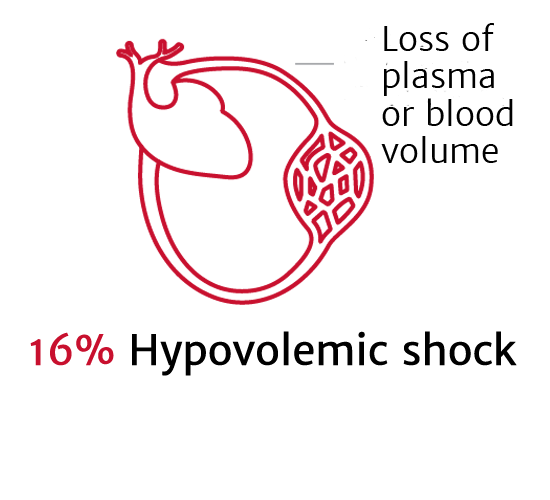
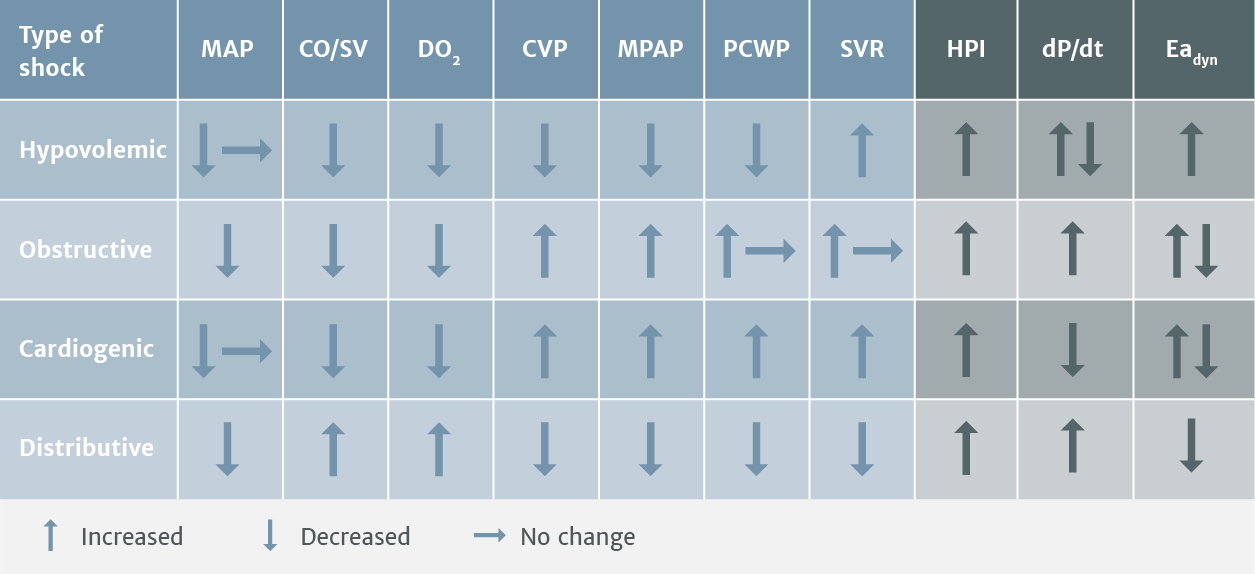
A primary reason for using advanced hemodynamic parameters for patients in shock, is to identify the type of shock in order to determine the most appropriate therapy.
Prompt identification is essential so that aggressive management can be started. Appropriate treatment is based on an understanding of the underlying pathophysiological mechanisms. 4
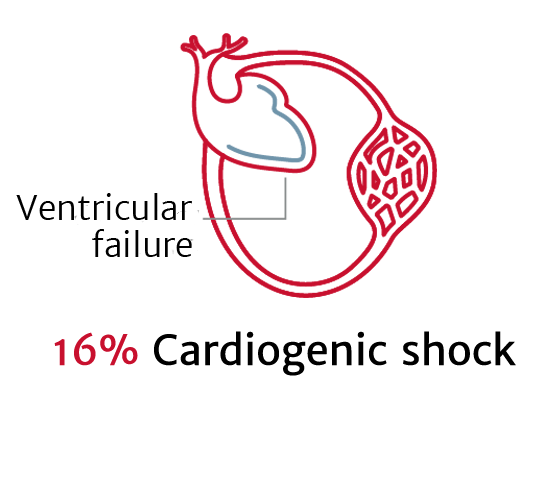
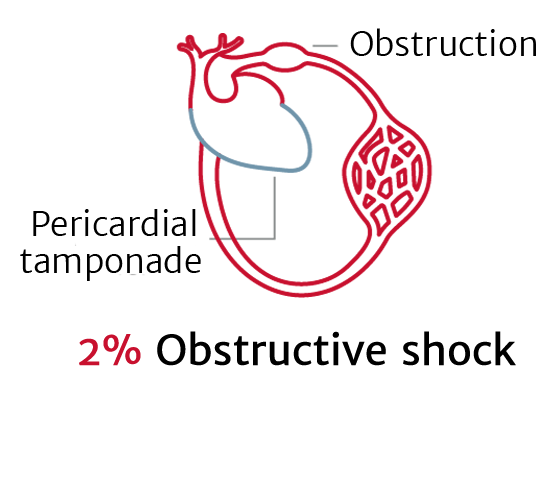
There are four primary types of shock: 2,4
Studies show that individuals with suspected similar diseases (such as heart failure, sepsis, and stroke) present with widely diverse hemodynamic profiles. 8
Trends in advanced parameters provide information on the underlying type of shock and enable clinicians to treat the specific type of shock more effectively.
Early, adequate hemodynamic support of patients in shock is crucial to prevent worsening organ dysfunction and failure. 4
Correcting arterial hypotension is essential to restore blood pressure and provide adequate cellular metabolism, which is the primary goal of resuscitation.
After correction of hypoxemia and severe anemia, cardiac output (CO) is the principal determinant of oxygen delivery and achieving a CO that is compatible with tissue perfusion is also critical.
Measurements of mixed venous oxygen saturation (ScvO2, SvO2) may also be helpful in assessing the adequacy of the balance between oxygen demand and supply. 4
Continuous measures and advanced hemodynamic parameters can be used to monitor the critically ill patient and provide additional insights compared to traditional parameters such as CVP, HR, and estimated volume loss alone.1 Shock situations can escalate quickly and advanced hemodynamic monitoring provides insights that enable you to make informed proactive clinical decisions.
Hemodynamic measurements, like those provided by the ClearSight system, FloTrac sensor, Acumen IQ sensor, or the Swan-Ganz catheter working with an advanced monitoring platform, can provide you insights into a patient's cardiovascular function to guide decision-making.
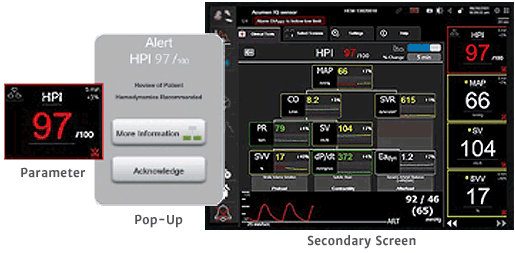
For a patient with shock it's important to monitor blood pressure for hypotension. A hypotensive event may be defined as MAP <65 mmHg for a duration of at least one minute. Blood pressure under this threshold may increase risk of mortality and organ failure.1
The Acumen Hypotension Prediction Index (HPI) software is a first-of-its-kind technology that detects the likelihood of a patient trending towards a hypotensive event before the event occurs. It provides you with insights to understand the root cause and inform a potential course of action for your patient. To learn more visit: Edwards.com/HPI.
Fluid therapy to increase cardiac output is an essential component of treating any form of shock and should be carefully monitored.4

Preload: the tension of myocardial fibers at the end of diastole, as a result of volume in the ventricle
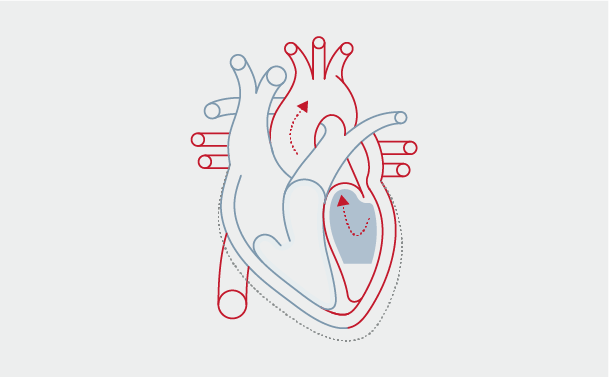
Stroke Volume (SV): volume of blood pumped from the left ventricle per heartbeat
Stroke volume measurement with Edwards devices, such as ClearSight finger cuff, FloTrac sensor, and Acumen IQ sensor, enable an individualized approach for administering fluid until SV reaches a plateau on the Frank-Starling curve, to help prevent hypovolemia and excessive fluid administration.
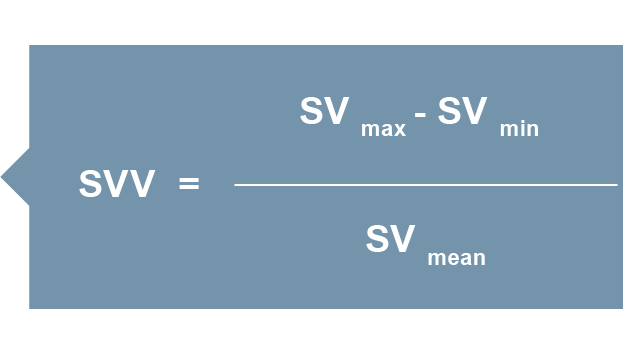
Advanced hemodynamic parameters such as SV and stroke volume variation (SVV), are key to optimal fluid administration and keeping patients in the optimal volume range. They are more informative than conventional parameters (such as blood pressure or central venous pressure) in determining fluid responsiveness and may help clinicians avoid excessive and insufficient fluid administration.
When managing perfusion, stroke volume can be optimized using the patient’s own Frank-Starling curve — a plot of SV vs. preload.
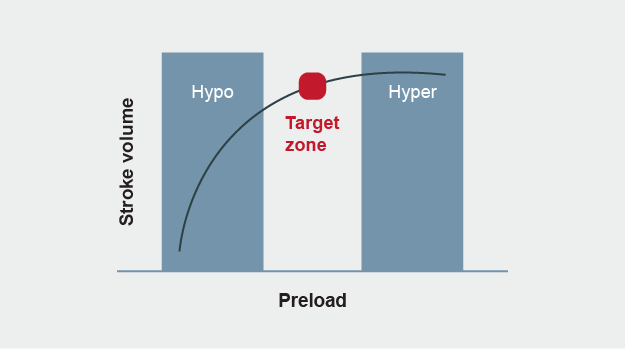
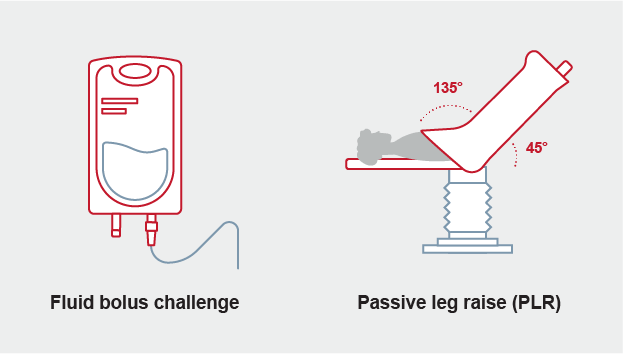
With the FloTrac sensor, Acumen IQ sensor, or ClearSight system, the patient’s location on his or her Frank-Starling curve can be determined by measuring ΔSV in response to change in preload using fluid bolus challenge or passive leg raise.
For control-ventilated patients, SVV has proved to be a highly sensitive and specific indicator for pre-load responsiveness, serving as an accurate marker of patient status on the Frank-Starling curve.
Edwards offers a range of clinical decision support solutions that provide advanced hemodynamic parameters used to manage critically ill patients.
We are committed to providing your institution, clinicians and staff with the highest levels of customer service and support to ensure seamless product implementation and ongoing use, including:
24/7 Technical support
For product information and orders
